- CVS officials said the company’s pharmacy benefit management division and Walmart were splitting over a price dispute Tuesday.
- The organizations walked back the announcement Friday.
- The split would have meant that many people who have CVS Health drug plans would no longer be able to pick up their prescriptions at Walmart locations.
Walmart and CVS Health’s pharmacy benefit management (PBM) division announced Friday they will continue to partner after resolving a pricing dispute, and it’s a “win” for consumers, health care expert Rita Numerof told The Daily Caller News Foundation Friday.
CVS twisted Walmart’s arm Tuesday with a relatively out-of-the-blue announcement of a pending split over prescription drug reimbursements.
The split would have meant that many people who have CVS Health drug plans would no longer be able to pick up their prescriptions at Walmart locations.
“With CVS and Walmart successfully reconciling their differences, they each win, and so do consumers,” Numerof told TheDCNF in an email statement. “Those that rely on Walmart’s convenient accessibility – especially in rural areas where other reasonable options may not exist – are the most notable winners. Quickly resolving this roadblock shows just how much of an impact this disagreement could have had on the patients they serve.” (RELATED: Sanders And Trump Could Become Strange Bedfellows In Fight Against High Drug Prices)
During the dispute, Walmart maintained that CVS was trying to control where customers filled their prescriptions, according to Bloomberg. Walmart has a reputation for making drugs affordable, including through its $4 generic prescription drug program.
CVS maintained that Walmart, which has leverage as one of the biggest pharmacy operators in the U.S., was pressing for higher reimbursements from CVS Caremark, its PBM subsidiary.

A pharmacist reaches for a prescription. Shutterstock image via Aleksandar Karanov
“Walmart’s requested rates would ultimately result in higher costs for our clients and consumers,” CVS Caremark President Derica Rice said in a statement Tuesday. “While we have enjoyed a long relationship with Walmart as a low cost provider in our broad national networks, based on our commitment to helping our clients and consumers manage rising pharmacy costs, we simply could not agree to their recent demands for an increase in reimbursement.”
CVS Caremark doesn’t just account for a portion of CVS revenue, it makes up most of its revenue, according to Bloomberg. More than 93 million Americans have CVS-administered prescription drug plans. The CVS-Walmart split would not have affected Medicare Part D beneficiaries or customers picking up prescriptions at Sam’s Clubs, according to the CVS statement.
PBMs like CVS Caremark often receive a bad rap because of their lack of transparency. Healthcare Finance News explains PBMs this way:
Pharmacy benefit managers are uniquely an American concept, acting as third-party administrators of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, and state government employee plans.
PBMs are often blamed for high drug prices. Senate Finance Committee Chair Chuck Grassley revealed his three-part initial plan to cut drug prices Wednesday. His plan did not include rethinking legislation surrounding PBMs, but he has discussed the need for oversight of them.
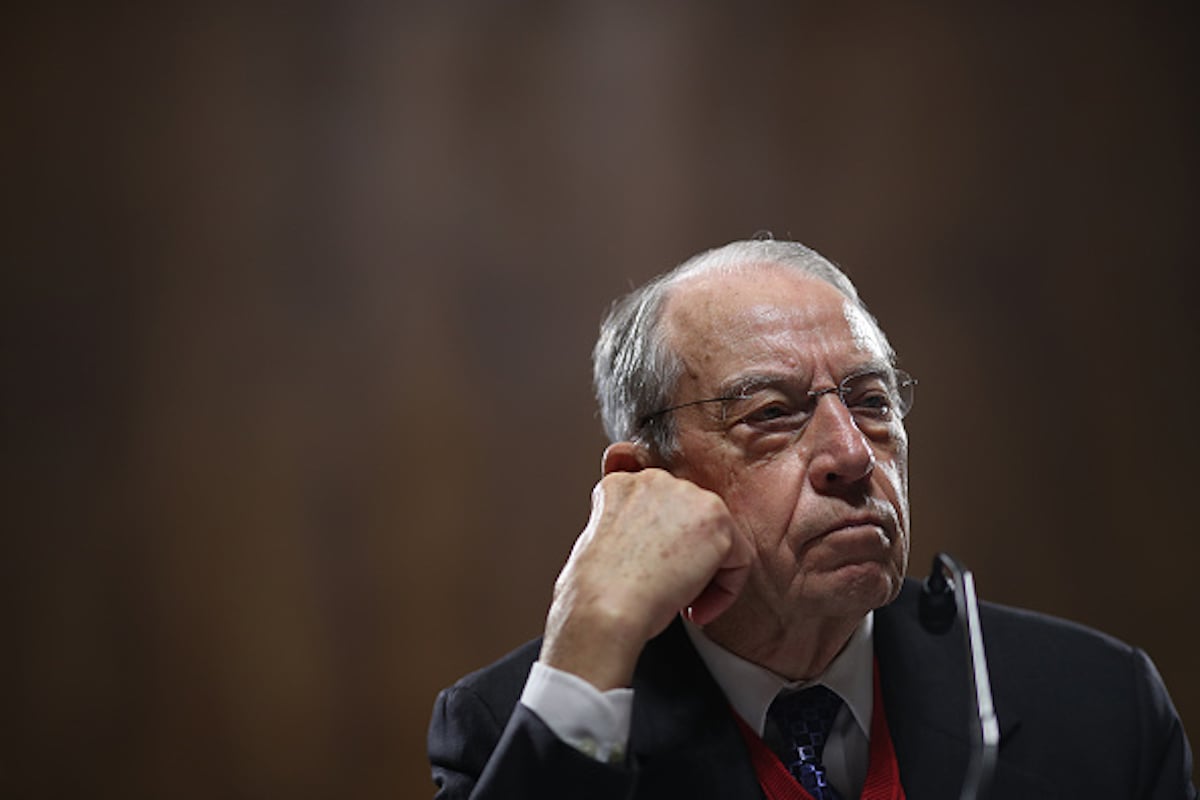
Senate Judiciary Committee Chairman Sen. Chuck Grassley attends a committee hearing on Capitol Hill November 15, 2018 in Washington, DC. (Photo by Win McNamee/Getty Images)
“I’ll also continue diligently pursuing oversight of both the public and private sectors of health care, including addressing health care consolidation and anticompetitive concerns, from supply chain middlemen to pharmacy benefit managers (PBMs) to hospitals and health insurers,” the Iowa Republican said in a Jan. 9 statement.
CVS was in the news for its health care business decisions back in 2018. CVS Health finalized a $69 billion acquisition of health insurance company Aetna on Nov. 28.
Numerof is the co-author with Michael Abrams of the 2016 book “Bringing Value to Healthcare: Practical Steps for Getting to a Market-Based Model.” Numerof and Abrams co-founded the health care consulting firm Numerof and Associates.
Follow Evie on Twitter @eviefordham.
Send tips to evie@dailycallernewsfoundation.org.
All content created by the Daily Caller News Foundation, an independent and nonpartisan newswire service, is available without charge to any legitimate news publisher that can provide a large audience. All republished articles must include our logo, our reporter’s byline and their DCNF affiliation. For any questions about our guidelines or partnering with us, please contact licensing@dailycallernewsfoundation.org.


